Hi everyone,
So when my kitten Marshmallow was 5 months old, we took her to the vet to be spayed. We were told that the spay (including anesthesia, medication, care, surgery, everything) would cost $275. We agreed that this was fine - we wanted top quality care for our baby girl and the money wasn't as important as getting her spayed. She had already had a check-up prior to this (with the same vet) and we were told she was perfectly healthy.
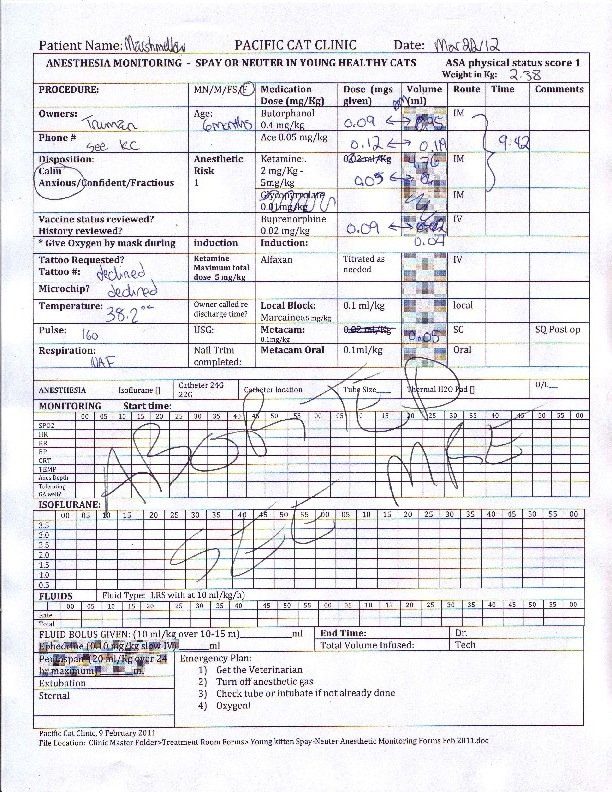
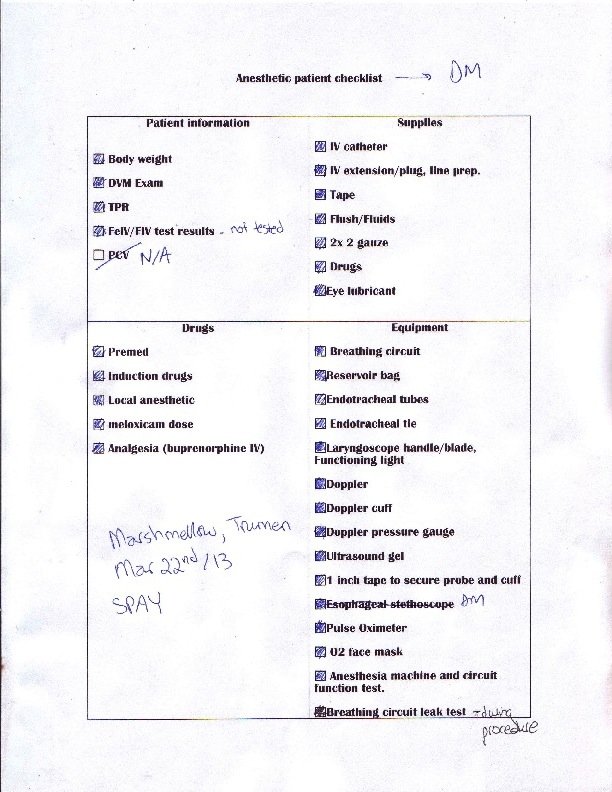
We dropped her off at the vet's (a clinic just for cats called Pacific Cat Clinic). Her being my little baby, I was so worried and upset to leave her, but I have had many cats in the past, and all of them had been spayed, so of course I left her in their good hands knowing it was the right thing to do. I was told they'd call me in the afternoon and I could pick her up in the evening. I went to university for my class and afterwards had a missed call from the vet's. Immediately my stomach dropped and I called them back, only to have them tell me that there had been an emergency and that they had to stop the spay surgery. I rushed home and spoke to the actual vet on the phone, who said that Marshie had stopped breathing/had "shuttered" breathing when they started her on the anesthetic and that her oxygen was too low, so they had to abort the procedure. They described it "like she was breathing with only one lung". I was horrified. They kept her in for observation until the afternoon, and we picked her up. Instead of the agreed upon $275, they charged us $400 because they said they had to call a specialist. Obviously, we were more concerned about our kitty than the money at the time, though looking back, I'm super upset that I had to pay extra for a botched procedure and now have an un-spayed cat. They didn't offer us any explanation for what had gone wrong in the surgery, and sent us home with no care instructions. Our baby was weird and didn't get back to normal for several days after that.
Since then, we have paid for specialist advice, as well as a $250 chest x-ray (which seemed to be normal), all trying to figure out what went wrong/if she has lung issues or heart problems. We could never find an answer. All in all, we paid about $1000 and got a failed spay.
Now, Marshmallow is a year and a half old and has gone into heat several times. It breaks my heart every single time because she is frustrated, we are frustrated, and when I ask for advice, everyone tells me to "get her spayed" and is very judgemental that she is still intact. I am afraid that if we try to get her spayed again, she will die from complications.
I don't know what to do. I want to do the right thing for her. I am so worried that if we try to get her spayed again, something will go wrong like last time. But on the other hand, if I don't get her spayed, she will have to go through heat for the rest of her life, and I have read about all the health complications (uterine cancers, etc.) that cats can get if they aren't spayed.
What should I do?
P.S. Marshmallow also showed an adverse reaction to shots/dewormer as well - at a previous checkup, she had a set of booster shots and some topical dewormer and spent the entire afternoon and night shaking violently. We had to check on her every hour throughout the night and were on the phone with the emergency vet hospital, who thought she was having a reaction to, or was sensitive to, the combination of shots and dewormer. So thought I would add this - it may be possible she is a super hypersensitive kitty who overreacts to many medical things - including anesthesia??
Thanks for any feedback anyone can provide! I'm so worried
Abby (and Marshmallow)
So when my kitten Marshmallow was 5 months old, we took her to the vet to be spayed. We were told that the spay (including anesthesia, medication, care, surgery, everything) would cost $275. We agreed that this was fine - we wanted top quality care for our baby girl and the money wasn't as important as getting her spayed. She had already had a check-up prior to this (with the same vet) and we were told she was perfectly healthy.
We dropped her off at the vet's (a clinic just for cats called Pacific Cat Clinic). Her being my little baby, I was so worried and upset to leave her, but I have had many cats in the past, and all of them had been spayed, so of course I left her in their good hands knowing it was the right thing to do. I was told they'd call me in the afternoon and I could pick her up in the evening. I went to university for my class and afterwards had a missed call from the vet's. Immediately my stomach dropped and I called them back, only to have them tell me that there had been an emergency and that they had to stop the spay surgery. I rushed home and spoke to the actual vet on the phone, who said that Marshie had stopped breathing/had "shuttered" breathing when they started her on the anesthetic and that her oxygen was too low, so they had to abort the procedure. They described it "like she was breathing with only one lung". I was horrified. They kept her in for observation until the afternoon, and we picked her up. Instead of the agreed upon $275, they charged us $400 because they said they had to call a specialist. Obviously, we were more concerned about our kitty than the money at the time, though looking back, I'm super upset that I had to pay extra for a botched procedure and now have an un-spayed cat. They didn't offer us any explanation for what had gone wrong in the surgery, and sent us home with no care instructions. Our baby was weird and didn't get back to normal for several days after that.
Since then, we have paid for specialist advice, as well as a $250 chest x-ray (which seemed to be normal), all trying to figure out what went wrong/if she has lung issues or heart problems. We could never find an answer. All in all, we paid about $1000 and got a failed spay.
Now, Marshmallow is a year and a half old and has gone into heat several times. It breaks my heart every single time because she is frustrated, we are frustrated, and when I ask for advice, everyone tells me to "get her spayed" and is very judgemental that she is still intact. I am afraid that if we try to get her spayed again, she will die from complications.
I don't know what to do. I want to do the right thing for her. I am so worried that if we try to get her spayed again, something will go wrong like last time. But on the other hand, if I don't get her spayed, she will have to go through heat for the rest of her life, and I have read about all the health complications (uterine cancers, etc.) that cats can get if they aren't spayed.
What should I do?
P.S. Marshmallow also showed an adverse reaction to shots/dewormer as well - at a previous checkup, she had a set of booster shots and some topical dewormer and spent the entire afternoon and night shaking violently. We had to check on her every hour throughout the night and were on the phone with the emergency vet hospital, who thought she was having a reaction to, or was sensitive to, the combination of shots and dewormer. So thought I would add this - it may be possible she is a super hypersensitive kitty who overreacts to many medical things - including anesthesia??
Thanks for any feedback anyone can provide! I'm so worried
Abby (and Marshmallow)